Primary Care, Workforce Planning
It’s all about the workflow: part one – reactive care
I have recently realised that the traditional terms of urgent care and routine care are not very helpful. How urgent exactly? Not urgent but a new concern – is that routine? So I prefer the terms reactive care - we respond to a new concern or need or request from a person/ patient. And pro-active care where we reach out to someone about their ongoing needs such as long term condition management or preventative services such a vaccination.
So what does good reactive care look like? Here are my thoughts:
1. Make it easy
People are busy, they have complicated lives with education, work, children, parents etc. Even if they have a serious health concern they still have other things they need to do. They are likely to be anxious if they are reaching out for help. Anxious about their health but also anxious about how they will be treated. So make it as easy as possible for them to get in touch with us. NEVER try to make it difficult in order to try and manage demand. It doesn’t work and it will just disproportionally affect those who need our help the most. Digital access is a really useful tool here but for some people picking up the phone or walking into the surgery to speak with someone will be easier for them.
2. Make it quick
Often we have a window of opportunity to help someone. If we are too late, things might deteriorate quickly. Things might also get better on their own, but even then we will have missed the opportunity to reassure and support someone at their time of need. Make it quick and our response can be simple and quick too. Delay and we can create even more work for ourselves
3. Make it kind
People will be nervous when they reach out to us. Nervous about their health and our response. So remember – we are not better than them, they are our equal and we are paid to look after them. Be kind, be human, be respectful, show compassion. It will make them feel better, will make you feel good and they will open up to you. Health outcomes are better when we are kind.
4. Be engaging
Not only should we assess people’s needs, but also their preferences for care:
- What do they think is wrong with them?
- Who do they think they should see, where, when and for how long?
Often people are right and even when they are not it is really helpful to know what they are concerned about, what their expectations are and what ideas they have about their likely condition and needs. Remember – the greatest untapped recourse in healthcare is the patient!
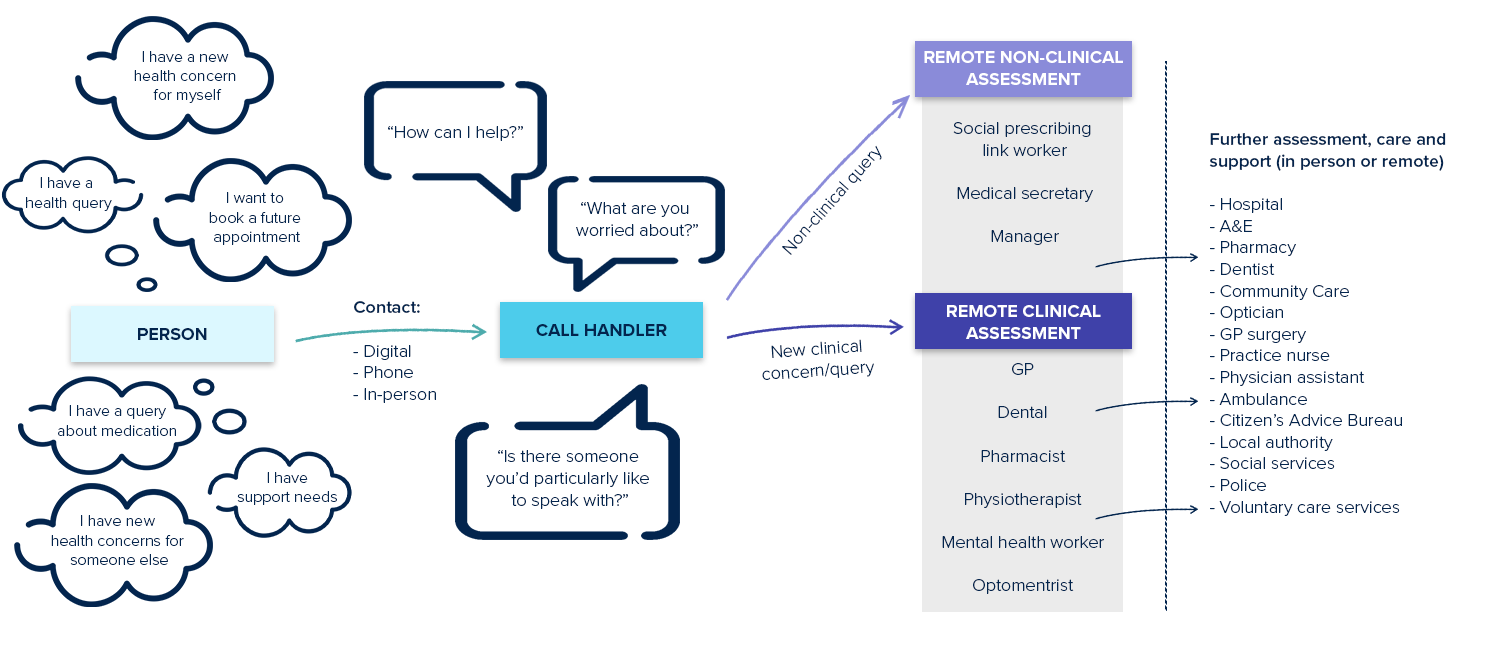
5. Be diverse
Primary care is a rapidly expanding team, use that diverse team to your advantage. Clinical pharmacists, First Contact Physiotherapists, Mental health Workers, Social Prescribing Link Workers, HCAs, nurses, GPs, Health Coaches, Dentists, opticians, the list goes on and is growing.
6. Be effective
Every chain is as strong as the weakest link. The first link in the primary care chain is the call/ message handler. This is the key step in the primary care pathway. This is where the pathway succeeds or fails. It is the most important job in primary care. And it’s not easy! Get this right and we make the best use of the most cost effective team in healthcare. Get it wrong and it works for no-one.
-
Let’s focus on the workflow and let’s invest in really effective “call handling”, it’s our greatest asset.


