Unlocking the value of ARRS for your Primary Care Network
The ARRS scheme was set up in 2019 to provide funding for thousands of additional roles within PCNs. There has never been more need for flexibility and personalisation within the NHS, but has the scheme helped with the vaccination programme? Is it helping create bespoke, multi-disciplinary teams?
We invited a group of health professionals to tell us how they make the best use of additional roles in a time of unprecedented demand. In this article, we share the key points and learnings from the webinar.
Dr Steve Laitner, GP and health consultant
Steve spoke about the value and benefits of additional roles in tackling population health inequalities and about how additional roles can help the community. When we think about healthcare and social care roles, he advises not to start with the roles, rather think about the needs of your patients and your community.
Steve recommends taking a broad view on additional staff requirements using a framework he’s developed:
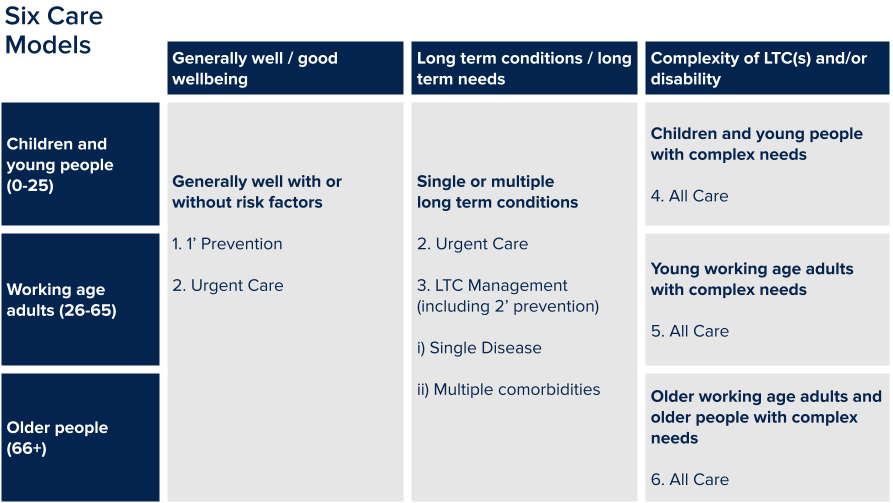
- Well people. This is a big area of demand. Look at prevention, immunisation, health checks, screenings.
- Primary prevention. Health coaches, nurses.
- Urgent care. GPs, paramedics, first contact physios, mental health workers.
- Long term condition management, which includes primary and secondary prevention – clinical pharmacists and nurses.
- Complex needs. Think about a holistic model that provides not only prevention and urgent care but continuity, proactive care, multi-disciplinary teams, clinical health coaching, anticipatory care.
So, Steve says, don’t start with the roles; start with a deep understanding of your community and your pressures and think about the additional roles that could help you in every area.
Dr Ruth Rankine, Director of Primary Care at NHS Confed
Ruth shared some of the most common ARRS challenges in her area:
Specificity of the roles
The narrow structure of the list of roles that PCNs can employ, job descriptions and bandings, makes the scheme feel too prescriptive. So how would you like it to change and what other roles do you envisage? Ruth believes that your wish list can be accommodated within the current scheme with some ‘outside the box’ thinking. She believes that there’s a real perception versus reality issue, and although it’s prescriptive it does have flexibility. A great example is a need for mental health support for patients. There’s a mental health practitioner role but it has limitations, so some PCNs recruit a social prescriber or health and wellbeing coach as a way of using the scheme flexibly.
Capacity
How many people are there in pools from which to recruit? We know there are shortages of some roles, for example in particular parts of the country, like the South West, it’s hard to recruit pharmacists. This is driving up costs as those pharmacists can ask for salaries that are beyond the ARRS scheme.
Ruth suggests focussing on collaborative working, which she knows is not always easy. Of course it’s easier to employ your own person than to work with the mental health trust to get the right person, but Integrated Care Systems play a key role in supporting PCNs with their workforce planning, making sure they get the right people.
Premises
This is a hot topic. Many ARRS roles have been recruited in the last 18 months to work from home. Now we’re getting back to face-to-face consultations, GPs are asking where on earth they can put these extra people. NHS England has a really helpful checklist for premises issues, with things to consider before you think ‘I need a new building’. Think about local opportunities, with local authorities or other parts of the NHS to use some of their space.
Training
Many ARRS roles were created to support the vaccination programme over the last year. These are often people new to healthcare who need effective supervision and support. Some social prescribers feel unsupported and want to leave. PCNs are really keen to make sure teams have the support to retain the roles. It’s not all down to the clinical director, others can also offer supervision and support. There are great examples of GP federations across the country who are filling ARRS roles with effective training and supervision.
Brenda Donnelly, Nurse and Clinical Director at South Southwark PCN
Brenda believes that to allow everyone to get joy from work, managers must treat the workforce like a garden, nurturing and watering people until they bloom.
Nature gives and nature takes. This has been a really difficult time for many people, especially at the start of the pandemic when teams pulled together under immense pressure. The vaccination programme is at last bringing hope and joy to PCNs, and ARRS roles are like the promise of a beautiful garden. Everything you might expect can be offered and is there to be discovered but it’s also vulnerable and prone to wilting and dying if it’s not nurtured and planted in the right place.
How the vaccination programme used ARRS
GPs and nurses are like the big trees in the garden. They know vaccines, but mass vaccination was new to them. Through ARRS they brought in new people including pharmacists, student nurses, medical students and retired GPs to help with vaccinations. The raft of skills was there, but there was a need for flexibility and agility to use them properly. People are not used to change, but actually vaccines were new to everyone and the programme was a real leveller.
The importance of wellbeing
Like a good garden, it takes investment and time to nurture people into new roles and new responsibilities. Good, healthy pairing is important. Putting young people who are great at IT with the vascular surgeon was a great ‘together learning’. It’s about investing in relationships, getting to know people and what drives them.
She spoke about her amazing social prescribers who came into the job not knowing what was going on, didn’t have the medical capacity to make decisions but became important parts of the team.
Brenda highlighted the importance of telling people how well they’re doing, giving them recognition, giving them a clap. She also highlighted the importance of paying people appropriately and on time and scheduling which works, using effective digital platforms rather than spreadsheets.
Dr Sachin Patel, GP Partner and Clinical Director, North West London
Sachin has put a lot of work into influencing colleagues to understand the vision of PCNs. He believes that understanding your own skillset in terms of what you’re good at doing and where you need support is critical to fostering positivity amongst the people you work with.
Sachin started looking at ARRS in 2016 when it was an NHS England pilot, even before PCNs, when there was not much funding and bringing in additional roles was a huge challenge. Initially people didn’t understand it but when they started building relationships, things started to fall into place.
Sachin agrees with Steve - start with the why. Sometimes you can’t convince everyone that the additional fee associated with ARRS is worth the spend. Understand and articulate the benefits which will resonate more with some colleagues than others but it’s important to explore and verbalise them.
The vaccine programme was a real change. PCNs on adrenalin that never stopped! Suddenly they were given a list of additional roles and they needed people, so they went into the community and found people who wanted to learn, to support and join in the hope of the vaccine programme and give back to their community. The biggest learning was understanding the value and skillset of people they recruited at breakneck speed.
The challenge was huge, they did 40,000 vaccines in a short time. Sachin expressed how valuable digital tools were for him. Working with Lantum helped them release the potential of the roles.
-
If you'd like to hear how Lantum is supporting PCNs across the UK to manage ARRS staff, please send an email to enquirires@lantum.com.


