NHS pressures and the need for innovation
The NHS will always be under pressure and, in the eyes of the service, will never have enough resources.
However, whilst resources are finite, so is healthcare demand — even though it doesn’t feel like it as demand outstrips capacity.
So what do we do?
First, it helps to think about the problems and solutions logically. I say problems plural, because there are a number of different issues, all with different solutions.
This helpful matrix sets out the different models of care(ing) required for different segments of the population and their unique needs.
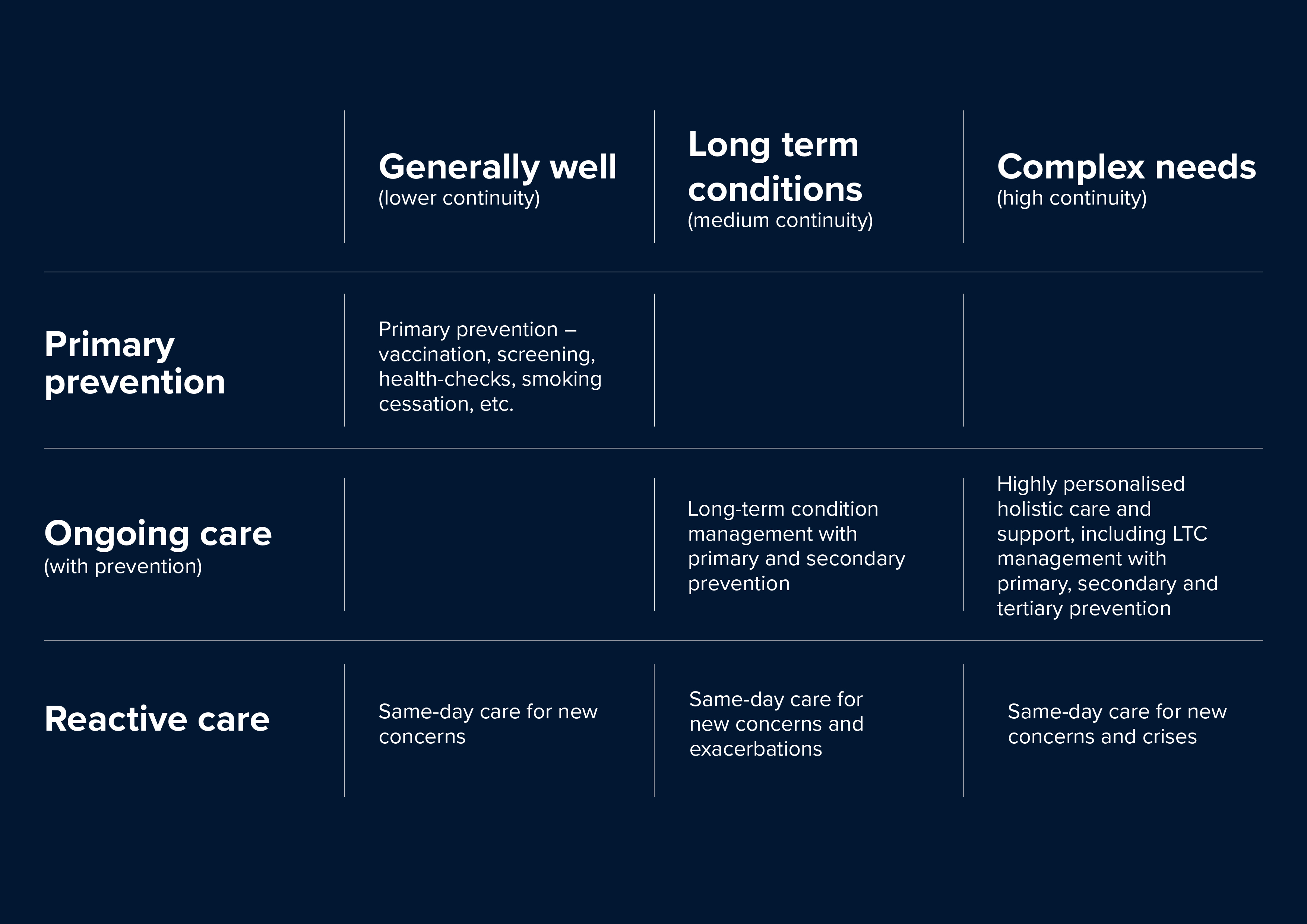
These models of caring can be summarised as follows:
- Primary prevention: Keeping people well through, for example, vaccination, screening, and health checks. Helping people to eat healthily, have a healthy weight, be physically active, not smoke and not drink too much. Includes targeted prevention for people at risk of developing long-term conditions.
- Long-term condition(s) care and support: Managing long-term conditions such as asthma, diabetes, heart disease and arthritis effectively and supporting people to self-manage as much as possible.
- Urgent care: Same-day access for new health concerns or exacerbations of long-term conditions. Diagnosing and treating urgent care needs and reassuring where appropriate, in a timely way.
- Complex needs care and support: Ongoing, proactive, holistic care with high levels of continuity for people who have a mixture of physical health conditions, mental health problems and social challenges such as disabilities, poverty, or social isolation. Includes rapid response for new concerns and exacerbations and crises. Likely to be delivered by a multidisciplinary team.
Managing winter pressure and pressures throughout the year is going to involve a segmented approach based on the categories above.
Personally, I would start with number four — complex needs care and support.
Work by HN in the Midlands has shown that just 5% of the population accounts for just over 70% of the Occupied Bed Days in local hospitals. Using data to identify this population early helps us provide targeted, proactive, holistic support for their complex needs and keep them at home for as long as possible.
Next, three — urgent care. GPs are especially good at dealing with undifferentiated demand from the public, which includes anything from mental health crises to breathlessness, abdominal pain and dizziness. Timely access is critical, and currently patients aren’t always able to access services quickly.
It’s not surprising that people call 111 or 999 and end up in A&E. Many times they’re admitted for something that a GP could have managed in a few minutes on the phone, aided by a trusting relationship and access to the patient’s lifelong medical record.
Then let’s tackle number two — care and support for long-term conditions. Good long-term condition care will help reduce the risk of exacerbations (and subsequent hospital admission).
Self-management support, medicine adherence and a robust care and support plan are essential requirements. There are some interesting start-ups in the technology support space (such as Aide Health) using conversational AI to help people monitor their condition and its treatment. When it comes to managing long-term conditions, nurses are the best.
And finally, one — primary prevention. They say prevention is better than cure, but in order to be able to invest in prevention we need to focus on all the other categories first, repair the leaks before the storm really sets in and help people to stay well. If we know they have risk factors for future long-term conditions, then we have to reach out to them with a compassionate offer of support. Never judge, always support!
So there you have it — four bite-sized chunks. They’re large chunks, but each has a suite of approaches to better manage specific needs and demands. It’s time to work with what we have, lean on what we know and start to tackle winter pressures head-on.
Remember: always start from the bottom up.
Lantum’s unique Connected SchedulingTM platform is designed to help healthcare organisations of all sizes understand their existing staffing resources, build centralised rotas quickly, and access extra locum support at a fraction of the cost of an agency.
To find out more about how Lantum can help your organisation build a stronger workforce while also saving time and money, get in touch with our team today.



